Les presento un artículo sobre este síndrome. Tiene mucha información importante. Está en inglés, el idioma principal en las publicaciones médicas.
Loffler Syndrome Clinical Presentation
medscape.com, updated Mar 05, 2014.
- Author:
Girish D Sharma, MD, FCCP, FAAP; Chief Editor: Michael R Bye, MDGirish D Sharma, MD, FCCP, FAAP Professor of Pediatrics, Rush Medical College; Director, Section of Pediatric Pulmonology and Rush Cystic Fibrosis Center, Rush Children’s Hospital, Rush University Medical Center.
- Coauthor(s)
Michael J Vinikoor, MD Fellow in Infectious Diseases, Department of Internal Medicine, University of North Carolina at Chapel Hill School of Medicine.
History
Symptoms of Löffler syndrome are usually mild or absent and tend to spontaneously resolve after several days or, at most, after 2-3 weeks. Cough is the most common symptom among symptomatic patients. It is usually dry and unproductive but may be associated with production of small amounts of mucoid sputum.
-
Parasitic infection
- Symptoms appear 10-16 days after ingestion of Ascaris eggs. A similar timeframe has been described for Löffler syndrome associated with N americanus, A duodenale, or S stercoralis infection.
- Fever, malaise, cough, wheezing, and dyspnea are the most common symptoms. Less commonly, the patient may present with myalgia, anorexia, and urticaria.
- Social and travel history should be carefully elicited to identify risk factors for exposure to parasites.
-
Drug-induced pulmonary eosinophilia
- Symptoms may start hours after taking the medications or, more commonly, after several days of therapy.
- Dry cough, breathlessness, and fever are common.
- Obtain a detailed drug history, including prescription and over-the-counter medications, nutritional supplements, and illicit drugs.
Physical
See the list below:
-
Usually, no abnormalities are found on physical examination. Cutaneous features of hypereosinophilic syndrome are described in a recent review article.[2]
-
Occasionally, crackles or wheezes may be heard on lung auscultation. Patients with drug-induced pulmonary eosinophilia commonly have crackles on physical examination.
Causes
See the list below:
-
Most cases of simple pulmonary eosinophilia are caused by parasitic infections or drugs; however, no cause is identified in one third of patients.
-
Parasites
- Ascaris lumbricoides (the most common parasitic etiology)
- Ascaris suum
- Necator americanus
- Strongyloides stercoralis
- Ancylostoma braziliense
- Ancylostoma caninum
- Ancylostoma duodenale
- Toxocara canis
- Toxocara cati
- Entamoeba histolytica
- Fasciola hepatica
- Dirofilaria immitis
- Clonorchis sinensis
- Paragonimus westermani
-
Agents in drug-induced eosinophilia
- Antimicrobials – Dapsone, ethambutol, isoniazid, nitrofurantoin, penicillins, tetracyclines, clarithromycin, pyrimethamine, daptomycin[3]
- Anticonvulsants – Carbamazepines, phenytoin, valproic acid, ethambutol
- Anti-inflammatories and immunomodulators – Aspirin, azathioprine, beclomethasone, cromolyn, gold, methotrexate, naproxen, diclofenac, fenbufen, ibuprofen, phenylbutazone, piroxicam, tolfenamic acid
- Other agents – Bleomycin, captopril, chlorpromazine, granulocyte-macrophage colony-stimulating factor, imipramine, methylphenidate, sulfasalazine, sulfonamides.
Laboratory Studies
The following studies are indicated in Löffler syndrome:
-
CBC count with differential
- Results show mild blood eosinophilia, usually 5-20%.
- Eosinophils may account for as much as 40% of the WBC differential in patients with drug-induced eosinophilia.
-
Stool examination
- Parasites and ova can be found in the stool 6-12 weeks after the initial parasitic infection.
- Pulmonary symptoms usually resolve by the time parasitic forms are found in the stool.
-
Immunoglobulin E (IgE) level: This may be elevated.
-
Analysis of sputum or gastric lavages: Larvae are occasionally found in sputum and gastric aspirates at the time of pulmonary symptoms.
-
Bronchoalveolar lavage: The eosinophilic count may be elevated.
Imaging Studies
See the list below:
-
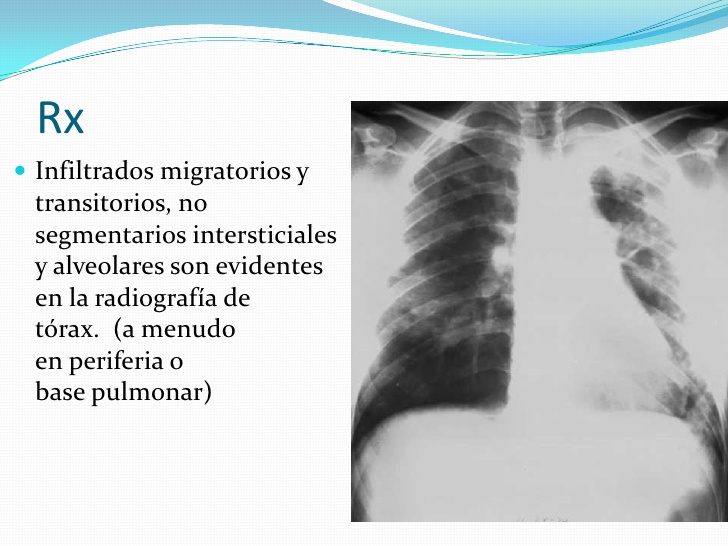
Chest radiography
 Initial chest radiograph of a 54-year-old man showing subtle opacity (arrows) in the right middle lung zone.
Initial chest radiograph of a 54-year-old man showing subtle opacity (arrows) in the right middle lung zone.  Follow-up chest radiograph of a 54-year-old man showing migrating opacity in the left lower lobe (arrows) obtained 20 days after the previous image.
Follow-up chest radiograph of a 54-year-old man showing migrating opacity in the left lower lobe (arrows) obtained 20 days after the previous image. See the list below:
- Roentgenographic abnormalities can be unilateral or bilateral.
- Most patients have peripheral densities, usually of a combined interstitial and alveolar pattern and often a few centimeters in diameter, although they may coalesce into larger areas of consolidation.
- Densities are generally transient, migratory, and disappear completely within 2-4 weeks.
- In drug-induced pulmonary eosinophilia, radiographic abnormalities resolve completely several weeks after withdrawal of the offending drug.
- Pleural effusions may be present in patients with nitrofurantoin toxicity. A case of eosinophilic pleural effusion with peripheral blood eosinophilia has been described with valproic acid administration.
-
Chest CT scanning: One report describes areas of ground-glass opacity (halo) around consolidation or nodules observed on high-resolution chest CT scanning. See the image below.
 High-resolution CT scan (1 mm collimation) obtained in a 54-year-old man showing consolidation with surrounding ground-glass opacity in the left lower lobe. Dilated airways are observed within the lesion. This CT scan was obtained between the first and second images above.
High-resolution CT scan (1 mm collimation) obtained in a 54-year-old man showing consolidation with surrounding ground-glass opacity in the left lower lobe. Dilated airways are observed within the lesion. This CT scan was obtained between the first and second images above. Procedures
See the list below:
-
Bronchoscopy and bronchoalveolar lavage
- These procedures are rarely indicated.
- In one report, the total number of cells found in bronchoalveolar lavage fluid (BALF) from patients with drug-induced pulmonary eosinophilia was significantly elevated compared to healthy subjects. Specifically, the number of lymphocytes and eosinophils in BALF was higher than in healthy subjects. These findings were not specific for drug-induced pulmonary eosinophilia because similar numbers were found in patients with chronic eosinophilic pneumonia. In addition to elevated eosinophils and lymphocytes in BALF, patients with acute eosinophilic pneumonia had high numbers of neutrophils in BALF.
Histologic Findings
See the list below:
-
Pathologic changes in the lungs have been described in patients who died from another cause while they concomitantly had simple pulmonary eosinophilia.
-
Eosinophilic infiltration occurs in the bronchi and bronchioles and in the alveolar and interstitial spaces. Parasitic forms are usually not found in the lungs.
Medical Care
Evaluation of Löffler syndrome can be conducted on an outpatient basis; inpatient care is not required.[5]
Surgical Care
Surgical care is not indicated.
Consultations
Pediatric pulmonologist
Diet
No special diet is required.
Activity
No activity limitation is indicated.
Medication Summary
The minimal nature of symptoms in most patients with Löffler syndrome usually denotes that no pharmacologic therapy is required for this self-limiting condition. For drug-induced pulmonary eosinophilia, discontinue administration of the offending drug. When a parasitic infection is documented, appropriate use of anthelmintic drugs is indicated. In severe cases of simple pulmonary or drug-induced eosinophilia, systemic corticosteroids are highly effective.
Corticosteroids
Class Summary
Markedly reduce the survival of certain inflammatory cells, including eosinophils. Eosinophil survival is dependent on the presence of certain cytokines (eg, interleukin-5 [IL-5], granulocyte macrophage colony stimulating factor and [GM-CSF]), whose effects are blocked by administration of corticosteroids.
Prednisone (Deltasone, Meticorten, Orasone, Sterapred)
May decrease inflammation by reversing increased capillary permeability and suppressing PMN activity.
Further Outpatient Care
See the list below:
-
Repeat chest radiography 4-6 weeks after initial presentation to document resolution of pulmonary infiltrates in patients with Löffler syndrome.
-
Repeat CBC count 4-6 weeks after initial presentation to document resolution of eosinophilia.
-
Examine stool for ova and parasites 6-12 weeks after initial presentation.
Inpatient & Outpatient Medications
See the list below:
-
Use appropriate antihelminthic therapy if parasitic infection is diagnosed.
-
Use systemic corticosteroids for patients with severe respiratory symptoms.
Complications
See the list below:
-
A case report describes hypereosinophilic syndrome with isolated Loeffler endocarditis, which resolved completely after 2 months of corticosteroid therapy.[6]
Prognosis
See the list below:
-
Prognosis is excellent.
Patient Education
See the list below:
-
Sanitary practice
- Educate people about sanitary disposal of feces, associated with educational campaigns for the use of latrines and pit privies in rural communities.
- Promote good handwashing technique to avoid ingestion of parasitic forms from contaminated soil.
-
In endemic areas of ancylostomiasis and strongyloidiasis, encourage use of proper footwear to avoid skin penetration of larvae of N americanus, A duodenale, or S stercoralis.
-
Avoid future use of the offending medication in patients with drug-induced pulmonary eosinophilia.
References- Kunst H, Mack D, Kon OM, et. al. Parasitic infections of the lung: a guide for the respiratory physician. Thorax. 2011. 66:528-36.
- Plotz SG, Huttig B, Aigner B. et al. Clinical overview of cutaneous features in hypereosinophilic syndrome. Current Allergy Asthma Report. 2012. 12:85-98.
- Shinde A, Seifi A, DelRe S, et al. Daptomycin-induced pulmonary infiltrates with eosinophilia. J Infect. Feb 2009. 58(2):173-4. [Medline].
- Janz DR, O’Neal HR Jr, Ely EW. Acute eosinophilic pneumonia: A case report and review of the literature. Crit Care Med. 2009 Apr. 37(4):1470-4. [Medline].
- [Guideline] Institute for Clinical Systems Improvement (ICSI). Diagnosis and treatment of respiratory illness in children and adults. 2008 Jan. [Full Text].
- Sen T, Ponde CK, Udwadia ZF. Hypereosinophilic syndrome with isolated Loeffler’s endocarditis: complete resolution with corticosteroids. J Postgrad Med. 2008 Apr-Jun. 54(2):135-7. [Medline].
- Abdul-Hadi S, Diaz-Bello Z, Zavala-Jaspe R, et al. Pulmonary paragonimiasis. Case report. Invest Clin. Jun 2008. 49(2):257-64. [Medline].
- Alberts WM. Eosinophilic interstitial lung disease. Curr Opin Pulm Med. 2004 Sep. 10(5):419-24. [Medline].
- Allen JN, Davis WB. Eosinophilic lung diseases. Am J Respir Crit Care Med. 1994 Nov. 150(5 Pt 1):1423-38. [Medline].
- Carroll JL, Sterni LM. Eosinophilic lung disorders and hypersensitivity pneumonitis. Taussig LM, Landau LI, eds. Pediatric Respiratory Medicine. St Louis, Mo: Mosby; 1999. 804-10.
- Corrin B. The lungs. Systemic Pathology. 3rd ed. London, England: Churchill Livinstone; 1990. 191.
- Cottin V, Cordier JF. Eosinophilic pneumonias. Allergy. 2005 Jul. 60(7):841-57. [Medline].
- Crofton JW, Livingstone JL, Oswald NC, Roberts AT. Pulmonary eosinophilia. Thorax. 1952 Mar. 7(1):1-35. [Medline].
- Das AM, Williams TJ, Lobb R, Nourshargh S. Lung eosinophilia is dependent on IL-5 and the adhesion molecules CD18 and VLA-4, in a guinea-pig model. Immunology. 1995 Jan. 84(1):41-6. [Medline].
- Fujimura M, Yasui M, Shinagawa S, et al. Bronchoalveolar lavage cell findings in three types of eosinophilic pneumonia: acute, chronic and drug-induced eosinophilic pneumonia. Respir Med. 1998 May. 92(5):743-9. [Medline].
- Katz U, Shoenfeld Y. Pulmonary eosinophilia. Clin Rev Allergy Immunol. Jun 2008. 34(3):367-71. [Medline].
- Kaufman J, O’Shaughnessy IM. Eosinophilic pleural effusion associated with valproic acid administration. South Med J. 1995 Aug. 88(8):881-2. [Medline].
- Kim Y, Lee KS, Choi DC, et al. The spectrum of eosinophilic lung disease: radiologic findings. J Comput Assist Tomogr. 1997 Nov-Dec. 21(6):920-30. [Medline].
- Lee HK, Jin SL, Lee HP, et al. Loffler’s syndrome associated with Clonorchis sinensis infestation. Korean J Intern Med. 2003 Dec. 18(4):255-9. [Medline].
- Ler WZ. Differential-diagnose der lungen infiltrierungen: er fle succedan-infiltrate (mit eosinophilia). Beitr Klin Tuberk. 1932. 79:368-92.
- Nadeem S, Nasir N, Israel RH. Loffler’s syndrome secondary to crack cocaine. Chest. 1994 May. 105(5):1599-600. [Medline].
- Neva FA, Brown HW. Intestinal nematodes. Basic Clinical Parasitology. 6th ed. Norwalk, Conn: Appleton & Lange; 1994. 113-51.
- Nogami M, Suko M, Okudaira H, et al. Experimental pulmonary eosinophilia in mice by Ascaris suum extract. Am Rev Respir Dis. 1990 May. 141(5 Pt 1):1289-95. [Medline].
- O’Sullivan BP, Nimkin K, Gang DL. A fifteen-year-old boy with eosinophilia and pulmonary infiltrates. J Pediatr. 1993 Oct. 123(4):660-6. [Medline].
- Ohnishi H, Abe M, Yokoyama A, et al. Clarithromycin-induced eosinophilic pneumonia. Intern Med. 2004 Mar. 43(3):231-5. [Medline].
- Pawlowski ZS. Ascariasis. Warren KS, Mahmoud AAF, eds. Tropical and Geographical Medicine. 2nd ed. New York, NY: McGraw-Hill; 1990. 369.
- Sharma OP, Bethlem EP. The pulmonary infiltration with eosinophilia syndrome. Curr Opin Pulm Med. 1996 Sep. 2(5):380-9. [Medline].
- Takafuji S, Nakagawa T. Drug-induced pulmonary disorders. Intern Med. 2004 Mar. 43(3):169-70. [Medline].
- Wang J, Palmer K, Lotvall J, et al. Circulating, but not local lung, IL-5 is required for the development of antigen-induced airways eosinophilia. J Clin Invest. 1998 Sep 15. 102(6):1132-41. [Medline]. [Full Text].
- Wong-Waldamez A, Silva-Lizama E. Bullous larva migrans accompanied by Loeffler’s syndrome. Int J Dermatol. 1995 Aug. 34(8):570-1. [Medline].
-
The most usual cause that people could read
out a blog post is always to know something fresh. Blog posts which include guides regarding tech, wellbeing and health, incremental processes, frequently gain a whole lot of
traffic. This really is only because people are searching instructions on how to
complete matters online every day. Daily, folks could read blogs
which tell stories that are interesting, good info,
or intrigue them in another way.
LikeLike